Nashville, Tennessee, 25 April 2025
Effects of sacro occipital technique (SOT) chiropractic and cranial therapy on dizziness in three patients 68, 72, and 75-years-old: A case series [Abstract]
Objective: To share a novel treatment for the care of three-patients presenting with unresolved 'non-pathological' dizziness.
Clinical Features: Three-patients, female age-75, female age-72, and male age-68 presented for care in my office with complaints of severe non-pathological dizziness. Medications and treatment for BPPV did not resolve their condition, which was ongoing for days to months.
Intervention/Outcome: Treatment consisted of sacro-occipital technique category-one prone block placement to treat pelvic torsion, cervical stairstep adjusting, and cranial techniques (e.g. internal temporal and external temporal bone adjusting on opposite sides, and sphenobasilar symphysis techniques). Whereas the patient had dizziness getting down on the table when it was time for them to get up, they were not dizzy and noticed their dizziness had resolved. The effects of this treatment appeared to last as within days the patients were no longer suffering from dizziness.
Conclusion: Current research into fascial continuity supports that pelvic torsion could be represented in the whole kinematic chain, even into the cranium and its dural-meningeal system. Compounded with visual and vestibular righting mechanism factors the process of righting the head to a 'pelvis in torsion' may have an adverse affect on the vestibular apparatus and subsequent dizziness.
Indexing terms: Chiropractic; SOT; dizziness; ageing; Category One blocking.
Cite: Benner C. Effects of sacro occipital technique (SOT) chiropractic and cranial therapy on dizziness in three patients 68, 72, and 75-years-old: A case series [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#BennerCaseSeries

Christine Benner DC, LAc, MS is is a 1989 graduate of New York Chiropractic College and a 2007 graduate of the Tri-State College of Acupuncture. She is the director of Oasis Healing Arts in New York City where she practices SOT Chiropractic and Acupuncture. Dr. Benner is a Certified SOT Practitioner as well as a Certified SOT Cranial Practitioner. Dr. Benner has been an SOT instructor since 1998, is chair of SOTO-USA’s board of certification, and a member of the board of directors for SOTO-USA.
Muscle activity in the head, face, and neck measured with surface EMG before and after cranial therapy: A case report of 2 patients [Abstract]
Narrative: Although it’s the most common type of craniofacial pain, very few practitioners in the world of dentistry or physical medicine know how to diagnose, let alone manage TMJ pain and dysfunction. Many claim to treat this joint, but with no real diagnosis other than the patient complaining of pain in the area, the vast majority of practitioners will throw their one or two catch-all 'TMJ treatments' at the problem, crossing their fingers in the hope that the patient feels better enough to not complain further.
When one thinks of craniofacial pain, it is commonly thought that most of the pain symptoms come from the muscles themselves, even if they are rarely the root cause. There are in fact reliable ways to measure muscle activity, and one such method is surface EMG. Muscles can be overactive or underactive, which can be accurately measured via the surface EMG analysis. In our small case study, although the chiropractor was confident that he was affecting the muscles and joints of the head and neck, he and his dental colleague decided to put this to the test by measuring muscles of the head, face, and neck before and directly after cranial therapy.
Although it was only performed on two patients, the results were compelling enough to warrant further study and a larger sample of patients. In regards to history, both patients experience various forms of craniofacial and cervical pain and dysfunction, and in their initial EMG scan both had muscle imbalances in almost all muscles tested. Immediately after receiving cranial therapy, almost all muscles that were misfiring (over or underactive) came back into the normal range.
This simple case study is significant for a few reasons. Firstly, very few TMJ treatments have had any research done validating their claims or results, especially utilising an independent and objective form of analysis. Secondly, no chiropractors and only a small minority of dentists utilise this form of analysis, and most will try and correct these muscle imbalances using TENS.
While TENS tends to work well on muscles that are overactive, it tends to create a worsening of symptoms and EMG scores in muscles that are underactive. It is also quite uncomfortable, difficult and time consuming to set up, and takes valuable chair time and manpower to implement. This leads me to the third reason this case study is novel and intriguing: the results strongly point to the importance of co-management in cases of TMJ pain and dysfunction.
A complex joint, it has the potential to create descending patterns of dysfunction on the rest of the body, is influenced by ascending influences as far away as the feet, and highly susceptible to maxillary underdevelopment (especially sagittal), myofunctional processes, and occlusion. By balancing the structures of the head and neck, and relaxing the muscles, the dental practitioner can then find a level a neutral plane on which to begin appliance therapy.
TMJ study is in its infancy, but given the prevalence of this condition and the current practitioner landscape that can only be defined as being akin to the 'wild west', any research into objective methods of addressing these dysfunctions are a welcome reprieve.
Indexing terms: Chiropractic; TMJ; surface EMG.
Cite: Scoppa J, Taylor R. Muscle activity in the head, face, and neck measured with surface EMG before and after cranial therapy: A case report of 2 patients [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#ScoppReynoldsSurfaceEMG

Jason Scoppa, DC, CSCP, CCSP, PAK has been practicing in the Seattle area since 2012. Having graduated from Palmer Chiropractic College in California, Dr Scoppa went on to earn post graduate certifications in SOT and SOT craniopathy through SOTO-USA, Applied Kinesiology through the ICAK, and Sports Medicine 1989 through the ACBSP. He has completed hundreds of hours of postgraduate coursework in the areas of TMJ, myofunctional therapy, airway, appliance therapy, expansion techniques, cranial facial growth and development, craniofacial pain, and and Cranial-Dental co-management.
Low back pain, genetics, and chiropractic preventative care: A longitudinal case study [Abstract].
Objective: To discuss how preventative chiropractic care might play a role in genetic related low-back pain.
Clinical Features: A 70-year-old female has been under chiropractic care for over 30-years. Both her parents and three siblings have all had multiple low-back and hip surgeries. While she has had some low-back and hip related issues, she is the only person in her family to receive chiropractic care, and in contrast to the rest of her family has been fully functional.
Intervention and Outcome: Monthly chiropractic care at this office utilised sacro occipital technique, soft tissue manipulation, and therapeutic exercise to improve kinematic chain balance and function. The patient is highly motivated and approximately 10-years ago began to include an active yoga practice along with her chiropractic care. While she has had some hip and low-back flare-ups she has been fully functional regularly riding her bicycle, hiking, and has been able to not need surgery.
Conclusion: Many of the low-back twin studies have demonstrated a relationship between hereditary/genetics and low-back pain. There may be a higher need for early chiropractic preventive care for the treatment of low-back/hip pain when there are heritable. familial characteristics.
Indexing terms: Chiropractic; SOT; LBP; heredity; active care; patient motivation.
Cite: Blum CL. Low back pain, genetics, and chiropractic preventative care: A longitudinal case study [Abstract]. Asia-Pac Chiropr J. 2025;6.2. https://www.apcj.net/SOT-Abstracts-2025/#BlumLBPGenetics
Charles L Blum DC, CSCP is in private practice Santa Monica, California and past president of SOTO – USA, now their research chair. He serves as Adjunct research faculty at Cleveland Chiropractic College and associate faculty at Southern California University of Health Sciences teaching the SOT Elective. Dr. Blum is a Certified SOT Cranial Practitioner, and on the peer review board of the Journal of Craniomandibular and Sleep Practice (CRANIO), Association of Chiropractic College Conference Peer Review Committee, Journal of Contemporary Chiropractic, Asia Pacific Chiropractic Journal, and Journal of Chiropractic Medicine. He has lectured nationally and internationally, has written various SOT related texts, compiled SOT and cranial related research, and has extensively published in multiple peer reviewed indexed journals and at research conferences from 1984 to the present.
Chiropractic treatment of a patient with chronic low-back pain followed over 20-years: A case report [Abstract]
Objective: To describe chiropractic treatment for a 40-year-old male patient presenting with chronic refractory low-back pain causing him to consider surgery and retirement from being a plumber.
Clinical Features: 40-year-old male patient presented over twenty-years ago with chronic low-back pain, unresponsive to medical interventions (e.g., medications, physical therapy, etc.), discopathy (MRI-determined), and told he would need surgery and retire from his plumbing career. He had significant bilateral lower-extremity muscle weakness and radiating pains as well as antalgic with reduced ranges-of-motion.
Intervention and Outcome: The patient was treated with sacro-occipital technique (SOT) block placement, spinal/extremity adjusting, chiropractic manipulative reflex techniques (non- musculoskeletal), and SOT/Van Rumpt cranial procedures. The patient was seen for 10-treatments over 2-months and was able to return to work and not need surgery. However over the past 20-years he has been seen episodically (1 - 3 times per-year) for flareups that resolve in 1 - 3 treatments.
Conclusion: This case discussed conservative chiropractic care for a patient with chronic low- back pain. Episodic care at 1 - 3 times per-year (1 - 3 office visits) over the past 20-years has allowed him to have a good quality-of-life, full activities-of-daily-living, and to not need surgery, while maintaining a plumbing career.
Indexing terms: Chiropractic; SOT; Chronic low-back pain; LBP; conservative care.
Cite: Boro WJ. Chiropractic treatment of a patient with chronic low-back pain followed over 20-years: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#BoroLBP20y
William J Boro, DC has been in private practice in Annapolis, Maryland for over 30 years. Dr. Boro uses sacro occipital technique, applied kinesiology, and Van Rumpt technique, in addition to using other standard methods of diagnosis, for the evaluation of structural, chemical and mental aspects of health. He is intent on increasing other doctor’s knowledge and understanding of how chiropractic is beneficial in cases other than strictly musculoskeletal problems. He has taught and presented papers nationally and internationally and looks forward to presenting more case studies in the future.
Chiropractic Manipulative Reflex Technique (CMRT): Considerations for uterine or
prostate treatment application for patients’ undergoing/undergone gender-affirming surgery and hormonal replacement therapy
Introduction: Chiropractic Manipulative Reflex Technique (CMRT) was developed by DeJarnette over the years of 1939 through 1981, with the last major update in his 1966 CMRT Text. During that period of time in our society discussions of a patient’s biological or identified gender designation was not generally discussed and contemplated by healthcare developers. Within our recent past there has been increased discussions about gender-affirming surgery (GAS) surgical procedures, that alters a person's physical appearance and sexual characteristics. These may also commonly include hormonal replacement therapy (HRT) to support the endocrine system. In light of these new considerations, the clinical question is, how might 'gender related' CMRT, prostate or uterine, be implemented for someone undergoing or having undergone GAS and related HRT?
Methods: A review of the various case studies of patients treated with CMRT suggested two specific studies that might worthy of consideration. One case study by Zablotney and Blum (1) noted a patient with situs inversus unresponsive to typical CMRT treatment. When an ultrasound of the patient’s abdomen was performed it was realised that she had situs inversus (sides of organ presentation were reversed). The doctor then reversed the sides of the body for treatment and reflex contacts, and the patient had a significantly positive response to the CMRT care.
Another case study by Blum (2) discussed a patient who had their gallbladder removed (cholecystectomy) and yet continued to have a form of phantom gallbladder referred pain, even though there was no gallbladder. Subsequent CMRT reflexes and manipulations were performed two weeks post-surgery and within 15 minutes of application the constant and unrelenting pain that had persisted pre and post surgery was relieved and 20 years later had not returned.
Results: Since discussing patients with GAS and HRT is a new consideration for doctors practicing CMRT we do not have research and evidence to adequately reach a confirmative decision. Therefore we must resort to biological plausibility and any possible related studies. With the two CMRT studies relating to situs inversus and phantom gallbladder referred pain it does seem reasonable that treating patients who have had GAS and HRT that the initial stage of care should focus on the patient’s biological birth presentation. If the patient does not respond as anticipated then modifying care to the patient’s current gender presentation may be indicated.
Conclusion: With new findings in healthcare it is always difficult for a healthcare practitioner to clearly know their path with therapeutic applications. Care that offers low risk and offers benefit are good platforms to further explore new vistas in therapeutic applications until we can have more information and evidence to better guide us.
Indexing terms: Chiropractic; CMRT; Gender affirming surgery; Hormone replacement therapy; Situs inversus.
Cite: Moore J, Blum CL. Chiropractic Manipulative Reflex Technique (CMRT): Considerations for uterine or prostate treatment application for patients’ undergoing/undergone gender-affirming surgery and hormonal replacement therapy. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#MooreBlumCMRT
Zablotney J, Blum C. Chiropractic care and the Situs Inversus patient: Modifying technique to match anatomy [Abstract only]. Asia-Pac Chiropr J. 2022;2.4.
Blum CL, Visceral Mimicry Syndrome and Cholecystectomy: A Chiropractic Case Study. Proceedings on the 2006 Conference on Chiropractic Research, Chicago, Illinois, September 15-16, 2006: 161-3.

Jeffrey Moore, DC graduated from Palmer December 1976. His first technique studied was Toggle Recoil from a student of Dr Herbert Himes and from Himes himself at times. He studied 'liquid crystals' and the Synchrotherm under Dr Andy Petersen. While he did the usual 'Palmer Package' course, he used SOT almost exclusively throughout college. He noted the Gonstead Club was noisy and the SOT Club at school seemed to be a bunch of quiet thinkers. He has practiced SOT throughout his practice life and yet acknowledges there is always much more to learn.
Visual cranial analysis: Palpation of the supine patient’s mastoid process position: An investigational study
Introduction: The field of chiropractic has various types of assessment tools used to pre and post evaluate the need for a therapeutic intervention and if that method was successful. This study looked at investigating visual cranial analysis as a method of assessing the structural and functional status of the cranial bones.
Clinical Considerations: Clinical applications have found that visual analysis has its strengths and limitations, especially in adults who have established bone growth in the cranium. The strength might be that position and shapes of the bones and their articulations show long-term patterns of tension and dysfunction. A weakness can be that commonly asymmetry in growth and development is not that unusual so a cranial bone may appear to be dysfunctional from a structural standpoint but functionally compensated.
Future Research: DeJarnette’s premise of Sacro Occipital Technique relates to a reciprocal movement of the cranium (occiput) and sacroiliac joint suggesting that these regions tend to mirror themselves as the bones positionally compensate for each other. With this concept in mind this investigator has observed with the placement of the index fingers under the mastoid tip of a patient in the supine position to almost always show a left finger inferior in position relative to the right. This occurs regardless of sacroiliac joint hypermobility or fixation, functional short leg, upper cervical or occipital subluxation or any other finding in the spine or extremities.
Conclusion: Further investigation is warranted to see why the same finding in the cranium would exist regardless of other findings in the body. What might be the cause of this finding and is there reliability between testers of different level of chiropractic palpatory experience?
Indexing terms: Chiropractic; SOT; mastoid process; visual assessment.
Cite: Tuttle D. Visual cranial analysis: Palpation of the supine patient’s mastoid process position: An investigational study. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#TuttleVisualCranialAnalysis

Daniel Tuttle, BA, DC, MSW, QEEG is both a Chiropractic Physician and Licensed Clinical Social Worker. He is a licensed QEEG Diplomate and has practiced Neurofeedback for 16 years. He led the first randomized control study on the effects of SOT chiropractic adjustments on the brain using qEEG analysis. He practices in Clearwater, Florida using both licenses to develop innovative methods of treating both the mind and body. Dr. Tuttle has extensive experience in treating patients utilizing SOT, cranial, and innovative TMJ treatment and assessment procedures.
Interdisciplinary care of a 15 year old male patient suffering from unresolving post-concussion syndrome symptoms secondary to high school American football trauma: A case report [Abstract]
Objective: To present chiropractic and cranial care of a 15-year-old patient suffering from unresolving post-concussion syndrome secondary to multiple head trauma while playing high school football (North American).
Clinical Features: A 15-year-old patient presented to this clinic having suffered a concussion 6-months prior describing multiple impacts to his body and head during a game. At his initial office visit he presented with unremitting headaches, photophobia, and hyperacusis unresponsive to rest, watching and waiting, and various medications.
Intervention/Outcome: The patient was treated with sacro-occipital technique prone block placement (category one) and adjustments to his cervical, thoracic, and cranial/TMJ regions. He was referred to a functional optometrist for vision exercises and dentist to balance TMJ occlusal and condylar function utilizing a mandibular appliance modified immediately after each chiropractic treatment. At one-month into care the patient’s symptoms were 80% improved, two- month mark 95% improved, and at the six-month mark had returned to playing football and full activities.
Conclusion: This case represents a 15-year-old male patient’s response to novel interdisciplinary care of his prior unresolving post-concussion syndrome symptoms. Further research is needed to determine what subset of pediatric patients with head trauma might be helped with this treatment model.
Indexing terms: Chiropractic; SOT; Category One blocking; prone; co-management.
Cite: Bloink TE, Blum CL. Interdisciplinary care of a 15 year old male patient suffering from unresolving post-concussion syndrome symptoms secondary to high school American football trauma: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2 www.apcj.net/SOT-Abstracts-2025/#BloinkPostConcussion
Thomas Bloink, DC, CSP, CSCP specializes in cranial-dental integration in Silicon Valley at the California Cranial Institute, which was founded in 1992. Dr. Bloink was on the board of advisors to help create SOTO USA and is actively involved in promoting the organization, presenting at research conferences throughout the world, and developing novel treatment approaches for functional neurological conditions. He works closely with many different specialists including dentists, orthodontists, and oral-maxilla surgeons. ENT's and others to ensure the best possible outcome for his patients.
Resolution of infantile brachycephaly, plagiocephaly, and torticollis without the use of a cranial remodelling orthosis: A case report [Abstract]
Introduction: In this paper I explore alternative treatments to the Cranial Remodelling Orthoses (DOC BandR, STARbandR) for nonsynostotic cranial deformation of infants.
Initial Presentation: Examination of 3-month-old revealed nonsynostotic brachycephaly with general flattening of occiput and specific flattening of the right occiput near lambdoidal suture. Posterior parietals were shoved superiorward creating a tall posterior cranium. Also noted was moderate plagiocephalic asymmetry with the right frontal, zygoma positioned anteriorward, and right lateral flexion torticollis.
Assessment: Lambdoidal restriction, especially right-sided, creating growth asymmetry of the occiput. Occipital flexion lesion (shortened AP distance, Falx Cerebri tension, high palate, especially right-sided) causing flat occiput and tall posterior parietals. Clockwise lateral strain of the Sphenobasilar junction causing plagiocephaly, torticollis.
Methods of Care: Treatment focused on releasing lambdoidal restriction, reducing sphenobasilar torsion, restoring occipital motion, redirecting cranial malpositions.
Results: At 9 months, full resolution of brachycephalic, plagiocephalic asymmetries, superior parietals, and torticollis.
Discussion: Proper assessment of the cause of the cranial deformity is key in determining resolution.
Conclusion: Improved research using measuring devices, better photography, and accessible training of infant cranial technique could advance the options of care for nonsynostotic cranial deformities.
Indexing terms: Chiropractic; SOT; Cranial Remodelling; plagiocephalic asymmetry; plagiocephaly.
Cite: Nichols K. Resolution of infantile brachycephaly, plagiocephaly, and torticollis without the use of a cranial remodelling orthosis: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#NicholsCranialRemodelling

Keila Nichols, DC has been practicing in the Northeast Dallas, Texas suburbs since 1989. She utilises traditional chiropractic techniques, including Sacro Occipital Technique, Craniopathy, Manipulative Reflex Technique (CMRT), as well as homeopathy and functional medicine. She enjoys functional medicine and spending any spare time with her husband and 5 'almost-adult' children.
Cranial Adjustments and Neurodivergent Children: Clinical Considerations [Abstract]
Narrative: The term 'neurodivergent children' can describe many types of the pediatric population including autism spectrum disorders, attention deficit/hyperactivity disorders, learning disabilities, such as dyslexia, dyscalculia, dysgraphia and dyspraxia, Tourette syndrome and other tic disorders, and sensory processing issues.
SOT cranial therapy can be vital in treating neurodivergent children. Getting motion in their cranium to help improve of cerebrospinal fluid circulation and glymphatic flow has clinically been shown to be very helpful for their condition. The actual treatment of children with autism spectrum disorder, especially those who have sensory processing sensitivity issues, can be very challenging.
Sensory processing sensitivity is found in the general population (approximately 20%) and colloquially called the 'Hypersensitive Person' discussed extensively by Elaine Aron. However children with autistic spectrum disorders will have an even lower threshold to stimuli so that they do not like their heads or bodies to be touched. It can be challenging for a child presenting with this condition to comfortably lie down on an adjusting table. Sometimes their body will be moving and they will be making loud noises so understandably this can make treatment very difficult for the doctor and patient.
Some treatment strategies can be having the parents let them look at an iPhone while they are being treated. Gentle pumping of the sacrum into flexion timed with inhalation can help reduce their motion and facilitate treatment interventions. The chiropractor has to try to synchronise their own movements with the children and treat them in any position possible. These positions can be while standing, sitting or even as they are twisting around on the adjusting table.
Even with the different patient positioning the same chiropractic techniques are applied for adjusting other children without their condition. Adjustments can be made either manually or with an activator type instrument to the child’s tolerance. It has been found that making sure to keep lights dim and no outside noises helps to calm them during treatment. These children do best with routines so try not to add too many things at each visit.
Conclusion: Realising that each neurodivergent child is different and may present with different sensitivities and body movements or preferences is important for chiropractors treating this patient population They are in great need of care that chiropractors can offer, but the chiropractor needs to accommodate the child as they present and not expect that the child has to change to meet the doctor’s needs or customary treatment methodologies.
Indexing terms: Chiropractic; SOT; Neurodivergent; paediatric; children; hypersensitive.
Cite: Cantwell K. Cranial Adjustments and Neurodivergent Children: Clinical Considerations [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#CantwellNeurodivergentChildren

Kathryn Cantwell DC, DICCP, CSP, CSCP, is a 1991 graduate from Western States Chiropractic College (University of Western States). She earned her paediatric Diplomate (DICCP) in 1996 and had been in practice in the Chicago suburbs for 24 years. Dr Cantwell is currently practicing in Beaverton, Oregon since 2015. She also is a Certified SOT and Cranial Practitioner (CSP, CSCP) and more than half of her practice is paediatrics and pregnancy. She also co-treats with many dentists treating TMJ and sleep disordered breathing issues.
Forty-hertz light and sound, gamma waves, and increased glymphatic circulation. Implications for cranial therapeutic approaches: A commentary [Abstract]
Objective: Objective: To discuss new findings on the treatment and prevention of Alzheimer’s disease and its implications on the possibility of enhancing cranial therapeutic approaches.
Commentary: Recently it has recently been discovered that light and sound that pulses at a 40-hertz frequency will stimulate gamma wave production in the cerebral cortex leading to increased glymphatic circulation. Generally glymphatic circulatory activities predominately occur when we are at sleep. Amyloid plaque build up in the brain has been attributed to incidence of Alzheimer’s disease and the current research is suggesting that increasing glymphatic circulation will reduce the plaque accumulation as well as prevent its deposition.
There are various types of devices being developed to help patients explore using 40-hertz light and sound frequency such as the utilisation of eye wear that flashes a light and has a plug for ear phones as well as iPhone applications that allow you to play memory games (e.g. Sudoku) on a screen that flashes at 40-hertz and makes an accompanying 40-hertz sound. It is likely in the near future we will see increased options that are more comfortable for patient usage, since improved glymphatic circulation has been demonstrating improved general cognitive function.
It is important to consider the issues of sleep deprivation in our aging population particularly those with airway compromise causing them sleep apnea or those with urinary track issues causing them to awaken regularly to urinate. It is possible that these complex issues are interwoven with adversely affecting the deep sleep necessary for gamma wave production and the necessary glymphatic circulation that helps with movement of fluid and reduction of plaque and catabolic end product build up in our brain and associated tissues.
Conclusion: Due to the low risk nature of the 40-hertz light and sound therapy this may be something worthy of experimenting with patients dealing with cognitive issues. This can be utilised while they are receiving cranial treatment as well as given to them for their home brain rehabilitative exercises. There may be issues with the flashing light with patients that have a history of epilepsy so we may see some contraindication considerations as this intervention becomes more widespread and accepted.
Indexing terms: Chiropractic; SOT; Alzheimer’s disease; glymphatic; light therapy; sound therapy; 40Hz.
Cite: Blum CL. Forty-hertz light and sound, gamma waves, and increased glymphatic circulation: Implications for cranial therapeutic approaches: A commentary [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#BlumGlymphatic
Charles L Blum DC, CSCP is in private practice Santa Monica, California and past president of SOTO – USA, now their research chair. He serves as Adjunct research faculty at Cleveland Chiropractic College and associate faculty at Southern California University of Health Sciences teaching the SOT Elective. Dr. Blum is a Certified SOT Cranial Practitioner, and on the peer review board of the Journal of Craniomandibular and Sleep Practice (CRANIO), Association of Chiropractic College Conference Peer Review Committee, Journal of Contemporary Chiropractic, Asia Pacific Chiropractic Journal, and Journal of Chiropractic Medicine. He has lectured nationally and internationally, has written various SOT related texts, compiled SOT and cranial related research, and has extensively published in multiple peer reviewed indexed journals and at research conferences from 1984 to the present.
Chiropractic care for a paediatric patient presenting with myoclonic seizures and delayed development: A case report [Abstract]
Objective: To share paediatric chiropractic care for a 9-month-old child presenting with myoclonic seizures (several dozen per day), delayed motor development, utilising G-tube since 6-week NICU stay.
Clinical Features: Induced delivery one-day after due date, suffered hypoxic ischaemic encephalopathy during birth, initial APGAR scores 2 and 1 respectively, required resuscitation, intubation, epinephrine administration, and penicillin treatment due to birth complications. The patient presented at this office with myoclonic seizures, multiple delayed development disorders, and one-month into care at this office diagnosed with cerebral palsy.
Intervention/Outcome: Pediatric sacro-occipital and cranial technique procedures were implemented 2-times a week for 8-weeks. By the sixth-office visit there was significant improvement in developmental functioning, removal of G-tube, and seizure intensity and frequency were notably reduced. Three-months into care (seen 1-time per week) the child was three-weeks seizure-free and beginning to start reaching developmental milestones.
Conclusion: This case illustrates the potential benefits of chiropractic care for paediatric patients with neurological and developmental challenges, highlighting the importance of paediatric chiropractors gently addressing structural misalignments and promoting neurological function.
Further research is needed to determine if regular paediatric chiropractic care may contribute to improved quality of life and functional outcomes in similar cases.
Indexing Terms: Chiropractic; SOT; myoclonic seizures; paediatric; developmental delay; paediatric cranial.
Cite: Rosen MG, Blum CL. Chiropractic care for a paediatric patient presenting with myoclonic seizures and delayed development: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#RosenMyoclonicSeizures
Martin Rosen, DC is a certified SOT®, SORSI, and SOTO-USA instructor, practitioner and craniopath as well as President Emeritus of SOTO-USA and the SORSI Research Board. He is a past instructor for the International Chiropractic Pediatric Association (ICPA), on the post graduate faculty of several chiropractic colleges, was a consulting member of the Committee for Chiropractic Practice and is on the editorial board for The Journal of Pediatric, Maternal & Family Health - Chiropractic.
Chiropractic care for a child presenting with autism, attention-deficit/hyperactivity disorder (ADHD), and retained primitive reflexes: A case report [Abstract]
Objective: To explore novel chiropractic care for a child presenting with autism, (ADHD), and retained primitive reflexes.
Clinical Features: A 7-year-old male patient was brought to this clinic by his Mother for supportive care. At age 4 he was diagnosed with autism and ADHD. His mother had to pull him out of school to homeschool due to his inability to follow directions, loud outbursts, inability to sit still and emotional dysregulation.
Intervention/Outcome: Due to his history, we proceeded with a general pediatric chiropractic exam and began testing for primitive reflex retention. The most notable retained primitive reflexes were the Moro reflex and Asymmetric Tonic Neck Reflex (ATNR). At the initial office visit he was treated with sacro occipital technique (SOT) category one (pelvic torsion with compromised sacral nutation) protocol and was also treated for occipital restriction. He was given specific home exercises to help integrate his care.
At his second office visit his Moro reflex had improved, however there was no improvement in the ATNR. His mother reported that he had not been performing the home exercises for the ATNR so the lack of improvement was attributed to this. On the 3rd visit, the ATNR was tested in both the standing and quadruped positions prior to treatment. Arm drift was found bilaterally in both positions. After treatment re-test showed moderate improvement in arm drift when turning to the Left, however no improvement when turning to the Right. While the patient was standing, more occipital release was performed and the ATNR was re-tested again. After performing the standing occipital release, the ATNR test was negative bilaterally in standing and quadruped positions. At the following visit, the ATNR was still negative when tested in both the standing and quadruped positions.
Conclusion: Chiropractic care for this patient appeared to have a positive effect on the child’s behaviour and Quality of Life (child and care givers). It appeared in this case that performing occipital release while standing rather than supine had a significant impact on the patient’s integration of the ATNR.
Indexing terms: Chiropractic; SOT; autism; ADHD; Category One; Moro reflex; Asymmetric Tonic Neck Reflex ATNR; Quality of Life.
Cite: Matson D. Chiropractic care for a child presenting with autism, attention-deficit/hyperactivity disorder (ADHD), and retained primitive reflexes: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#MatsonADHD

Diana Matson DC, CSCP is a graduate of Palmer West, where her foundational interest in Sacro Occipital Technique (SOT) and integrative care through collaboration with other healthcare providers took root. Diana currently practices in the scenic Sacramento foothills of California. Her love of yoga and trail running have cultivated a passion for movement that naturally extends into her patient care. She specialises in treating children and young adults, employing both SOT and SOT cranial techniques. A key focus of her approach involves the integration of breath-work and primitive reflex patterns to support optimal health and development.
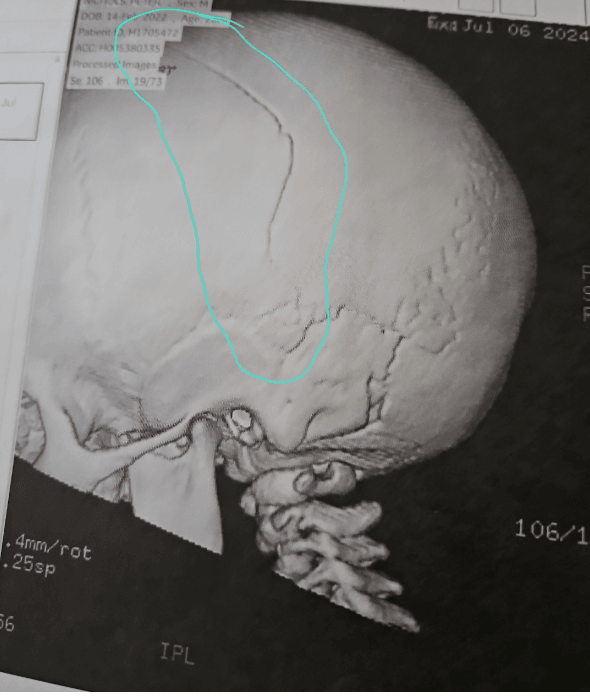
Correction of dramatic cranial changes after traumatic impact on a 2-year-old: A case report [Abstract]
Introduction: This case report describes the application of cranial techniques to correct dramatic cranial changes presenting in the cranium of a 2-year-old after sustaining severe blunt-force trauma to the left parietal (See Figure below)
Initial Presentation: Patient presented with a fractured left parietal bone secondary to receiving a blow to the top of his head from the full weight of a 10-foot pressure-treated 4x4 board (~70lbs, 31kg). Patient had been taken to the Emergency Room where Tylenol was administered, and a CT was taken after 3 hours of observation and then patient was released. The patient did not lose consciousness but experienced some confusion, difficulty with balance, and difficulty speaking for 4 days post-impact.
Assessment: Assessment of Neurological Deficiencies showed reduced ability to speak (slurring) and reduced ability to balance (unable to stand unassisted). The front portion of his parietal bone appeared to have been pushed inferior beneath the temporal bone, which in turn had flared laterally and inferiorly.
Methods of Care: Treatment focused on lifting the front portion of the parietal bone and de-rotating the left temporal bone. In addition, treatment worked to maintain flow of CSF.
Results: Fracture has fully healed. Ear flare difference is imperceptible. Head shape is equal and symmetrical. No lasting verbal or cognitive impairment.
Discussion: Addressing mechanical displacement of cranial bones in the acute stage of care alleviated verbal impairment and allowed for a symmetrical and functional healing of cranium.
Conclusion: Cranial techniques can be gentle enough and powerful enough to be used on a fractured cranium to allow for full healing in a young child.
Indexing terms: Chiropractic; cranial; parietal fracture; head injury.
Cite: Nichols J. Correction of dramatic cranial changes after traumatic impact on a 2-year-old: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#Nichols2yoPostTrauma

Jesse Nichols, DC is a second generation Chiropractor and is a recent graduate from Parker University. His chiropractic college studies focused on post-partum sacropelvic recovery, and organizing SOT mini-seminars, supporting the SOT club and SOT elective class. He is currently taking a deep dive into studying sacro occipital technique (SOT) being mentored by his mother Keila Nichols, DC who has been a long time teacher and practitioner of this method of care.
Chiropractic care of a 7-year-old male child presenting with resolving encopresis: A case report [Abstract]
Introduction: The purpose of this case report is to share the chiropractic care of a 7-year-old male brought to the clinic by his grandmother with a chief complaint of encopresis for three years and learning difficulties. The condition caused significant distress for both the child and the family, affecting the child’s social, emotional, and psychological well-being, causing him to feel embarrassed and humiliated. This patient had not been seen by another health care provider for this condition prior to being seen at this clinic.
Methods/Intervention: Based on the postural, cranial, neurological and Sacro Occipital Technique (SOT) assessment he was categorised has have a category two (posterior sacroiliac joint instability) with cranial stress and imbalance. He was treated as a category two with the cranial 'basic two' procedure, treated for sphenobasilar symphysis cranial strain imbalance as well as with trans cranial therapy (TCT) low level laser.
Results: The child’s step-mother brought him in for a follow-up appointment two weeks later and reported that the patient has not had a single accident since his first adjustment and the two weeks was the longest period of time for him without having an accident. It was recommended that he return for care if there were any flare-ups or possibly for maintenance care. However since his second office visit the child has not returned for care at this office and it is presumed at this time that his condition has remained stable.
Conclusion: It was compelling that prior to care his condition had been stable and unresponsive to watching and waiting, patient attempts to control his behaviour, and the use of laxatives. It is unclear what the specific mechanism might have been that helped this child and they could have been from reducing pelvic imbalance, improving cranial function, and stress reduction which may have had psychogenic contributions to his condition.
Indexing terms: Chiropractic; SOT; encopresis; Category Two; cranial.
Cite: Erickson J. Chiropractic care of a 7-year-old male child presenting with resolving encopresis: A case report. [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#EricksonEncoparesis

John Erickson, DC is a 1997 graduate of Palmer Chiropractic College, Davenport. He and his lovely wife Michelle have six children. His practice in in Loveland, Colorado and incorporates a multidisciplinary approach, currently incorporating sacro occipital technique (SOT) and SOT cranial techniques. Dr Erickson delivered his first research presentation at last's SOT Research Conference and continues to contribute.
Successful Sacro Occipital Technique care for an 11-year-old female presenting with scoliosis: A case report [Abstract]
Introduction: An eleven-year-old female diagnosed with scoliosis by her allopathic paediatrician at her yearly check-up presented at this office for care. Because her family was treated at this office for years her mother brought her in for a second opinion. Her initial assessment indicated that she did have a scoliosis with a convexity to the left in the lumbar region and to the right in the thoracic region.
Intervention: The patient was initially treated as a category two and was blocked in the supine position until her indicators subsided and was treated with a DeJarnette scoliosis protocol presented in his 1969 Chiropractic Assistant’s Manual. The patient had a scoliosis with the lumbar convexity towards the left and the thoracic convexity towards right. So she was treated initially supine with a pelvic block placed at a 45° caudal angle through the right acetabulum and another pelvic block placed under her shoulder at a 45° caudal angle towards her spine.
As her body relaxed she was then turned to the prone position and blocks were placed at a 45° caudal angle bilaterally through her ASIS (SB+ block position). Once blocks were placed and the patient relaxed, simultaneous pressure was gently applied to reduce the increased asymmetrical muscle tension at the concavity of the curves (case lumbar concavity on the right and thoracic concavity on the left). After the muscle tension was reduced then thumb pressure was applied to the convexities in the lumbar and thoracic region simultaneously until the vertebral spine felt like it relaxed into a more symmetrical positioning.
Outcome: Following the first office visit she was seen again eleven days later and the scoliosis was improved but still present. She was treated again three weeks later and at that time there was no sign of the scoliosis. At a five-week follow up office visit her scoliosis was back but not as severe as initially. She was then seen once a month over two months with no trace of the scoliosis. At seven month from instituting chiropractic care her scoliosis returned though was very mild, but following that treatment it never recurred. When she had her twelve-year-old check up from her patrician there was no sign of any scoliosis.
Conclusion: This case presents treatment of an adolescent with scoliosis diagnosed initially by her paediatrician and treated successfully with sacro occipital technique protocols. It may be of value for future studies investigating more interdisciplinary relationships between allopathic and chiropractic physicians treating children with scoliosis.
Indexing terms: Chiropractic; SOT; blocking; scoliosis.
Cite: Simmons DW. Successful Sacro Occipital Technique care for an 11-year-old female presenting with scoliosis: A case report [Abstract]: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#SimmonsScoliosis

David Simmons, DC took his first seminar from Dr. DeJarnette in 1978. He has been teaching sacro occipital technique (SOT) at the SOT clubs at Cleveland Chiropractic College – Los Angeles and Southern California University of Health Sciences, as well as SOT Regional Certification Series in Los Angeles, California for over 28 years. He is passionate about practicing chiropractic and loves to go to his office six days a week working to help patient improve their health through natural means.
Unexpected resolution of chronic sinus headaches following chiropractic care for cervicogenic headaches: A case report [Abstract]
Objective: To discuss chiropractic management of a patient presenting with suboccipital headaches and chronic allergy-induced sinusitis.
Clinical Features: A 50- year-old female with a history of chronic sinus headaches presented with constant bilateral suboccipital pain for 3 weeks. The patient has had sinus headaches 1 time per week for most of her adult life. She managed the symptoms with daily over-the- countermmedications. The physical examination was unremarkable, revealing no red flags. This episode of suboccipital headaches was previously treated with stretching and massage without resolution; she received diversified-type chiropractic care 6 months previously without change to conditions.
Intervention and Outcomes: Upper cervical specific radiographs were used for Atlas Orthogonal (AO) biomechanical analysis. The patient was scheduled once/wk for 4 weeks and adjusted as indicated using AO, Thompson, and sacro-occipital technique assessments. Suboccipital headaches resolved after 3 treatments. The patient noted that sinus headaches had also ceased. She chose to discontinue her routine antihistamine use; her allergy symptoms have not returned.
Conclusion: Chiropractic care is a validated option for management of cervicogenic and tension-type headaches. This patient experienced improvement in concurrent allergies and/or sinus headaches. Further research is needed regarding upper cervical specific correlation.
Indexing terms: Chiropractic; SOT; AO; tension-type headache; sinus headache; allergies; upper cervical specific.
Cite: Hagen C, Mansholt B. Unexpected resolution of chronic sinus headaches following chiropractic care for cervicogenic headaches: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#HagenMansholtCervicogenicHeadaches

Chad Hagen, DC is is a 2005 Palmer graduate and second generation chiropractor. Classically trained in Atlas Orthogonal and a Certified SOT® Instructor, Dr Chad’s private practice specialises in these techniques located in Bettendorf, Iowa. As Assistant Professor at Palmer Davenport, Dr. Chad teaches in both the Technique and Philosophy Departments. His instructional focus is Subluxation Analysis, Toggle Recoil, Chiropractic Theory, and both the Sacro-Occipital Technique electives. Dr Hagen is also Advisor for the SOT and Palmer Upper Cervical clubs.
Focal nodular hyperplasia of the liver incidentally identified in a chiropractic patient with rib pain: A case report [Abstract]
Objective: To describe an adult male with focal nodular hyperplasia (FNH) of the liver mimicking right lower rib pain.
Clinical Features: A 42-year-old male presented with right lower rib pain extending from the mid-sternal to the mid-axillary line. The pain was sharp, aching, and radiating. He had a history of liver laceration after blunt abdominal trauma 34 years prior.
Interventions/outcomes: Murphy’s sign was positive, and there was reduced and painful right lateral thoracic bending. Palpation of the anterior right lower ribs elicited epigastric pain. An Activator™ instrument-assisted adjustment was performed on rib 8, which did not relieve the pain.
The working diagnosis was intercostal neuralgia. The patient was referred for a sonographic examination of the gall bladder to discard acute cholecystitis. The sonogram revealed an incidental large hypervascular liver mass. Multiphase contrast abdominal computed tomography was performed to further characterise the lesion, demonstrating a mildly hyper-attenuating, and moderately enhancing 8.8 cm mass in the left lobe of the liver, with hypo-attenuating central scar, consistent with FNH.
Conclusion: Remote trauma may predispose patients to developing painful visceral lesions that mimic musculoskeletal pain. Diagnostic imaging plays a crucial role in securing the diagnosis and directing appropriate management.
Indexing terms: Chiropractic; SOT; intercostal neuralgia; cholecystitis; liver; referral.
Cite: Guzman IMR, Halverson J. Focal nodular hyperplasia of the liver incidentally identified in a chiropractic patient with rib pain, a case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#GuzmanLiver
Ibis Melissa Roman Guzman DC is a graduate from Life University, with a Master’s in Environmental Risk Management and Assessment and a Bachelor’s in Biology with a concentration in Microbiology. Currently, she is a professor at the Universidad Central del Caribe and a chiropractor at the Hospital Regional de Castañer, having previously worked at Hospital Pavía de Arecibo as part of an interdisciplinary rehabilitation team. She is the founder and owner of Ibis Family Chiropractic, LLC, where she provides evidence-based chiropractic care. Additionally, she has conducted research on environmental microbiology and molecular techniques in collaboration with international academic institutions, with publications in scientific journals and presented at ACCRAC 2025.
Chiropractic treatment of a 33 year old female presenting with bilateral toe walking and mild scoliosis throughout entire spine: A case report [Abstract]
Objective: The objective of this report is to share novel treatment for a toe walking in a 33-year-old female presenting with a life-long toe walking condition.
Clinical Features: A 33 year old female (now 35 years old) presenting for chiropractic care with unresponsive bilateral toe walking and mild scoliosis in her entire spine due to gait disturbances, to an interdisciplinary clinic having given up on other options (e.g., surgery, physical therapy, etc.).
Intervention and Outcome: Treatment consisted of sacro-occipital technique, cranial techniques, and one visit to a pelvic floor physical therapist to address spinal/coccyx, lower extremity, and postural imbalances, likely related to the patient’s life-long toe-walking. After two-months of one-two chiropractic treatments per-week the patient was able to stand flatfooted with some forward torso bending for the first time in her life. Her gait still consisted of toe-walking but had some intervals of heel-toe walking as well. After eight-months of chiropractic treatments, approximately one treatment per-week, she has attained proper gait mechanics and only toe- walks out of habit on occasion.
Conclusion: This case demonstrates a conservative treatment for an adult patient presenting with toe-walking/gait disturbance when other methods were not effective.
Indexing terms: Chiropractic; SOT; adult toe-walking.
Cite: Stowell LM, Blum C. Chiropractic treatment of a 33 year old female presenting with bilateral toe walking and mild scoliosis throughout entire spine: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#StowellToeWalking

Lisa M Stowell, DC focuses on the safest and most natural approach to chiropractic care utilising cutting edge techniques such as SOT (sacro-occipital technique). She incorporates 'Food First' as part of her approach to customise personal dietary needs as well. Besides head, neck and low back pain, Dr Stowell addresses conditions such as diabetes, fibromyalgia and even depression and fatigue. Dr Stowell has been published in an international, peer-reviewed chiropractic journal as well as accepted for presentation at 2024 ACC-RAC Conferences.
Chiropractic care for a patient preparing for a Norwegian Trek when she couldn’t walk up stairs: A case report. [Abstract]
Objective: To present a case report on a 68-year-old female unable to walk up stairs without using her arms in distress due to a planned vacation involving hiking who was successfully treated with chiropractic care.
Clinical Features: A 68-year-old female presented for care at this office complaining of relatively severe pain in her left elbow beginning three weeks prior which does not allow her to use her left hand. A more urgent complaint to her was her chronic worsening of extreme weakness in her both her hips and oedema in both her ankles. She was deeply concerned because had a 'trek' in Norway coming up and she needed to be able to hike though now due to her weakness struggles to walk up stairs and needs to pull herself up with her arms using side rails. The patient reported a past history of a right ankle fracture 8 years prior and had only minimal physical therapy with no supervision following the injury.
Intervention and Outcome: The patient’s hip and lumbar ranges of motion were difficult to assess due to her apprehension and muscle weakness. Arm fossa test positive indicative of a posterior sacroiliac joint hypermobility syndrome with pelvic torsion. Assessment of her upper left extremity found that she had a left humeral head was anterior displaced and her left radial head posterior subluxation. She was treated with chiropractic care that included sacro occipital technique category two block treatment, therapeutic massage, orthopaedic blocking, Activator™ instrument, and her extremities were also adjusted.
At second visit two days later the patient reported she had regained the use of her left hand though she continued to have achiness in the left elbow but did not limit her movement. She noted that her hips felt stronger as well but the right hip continued to feel like it was 'catching'. Following the first office visit she reported that her 'hip' felt better for about two hours but she felt it destabilise while standing when shopping. She also noted that the oedema in ankles had resolved. On the second office visit the category two basic cranial was performed while she was being treated supine with pelvic blocks. She was also given home exercises to strengthen and rehabilitate her gluteus medius muscles.
By the third visit she was able to walk up the stairs without using her arms. Her left shoulder and elbow were significantly improved with only tenderness at left elbow that were treated with adjustments and ultrasound therapy. She was seen three times for the first week, then two times per week the following week, with one more treatment the third week at which time she felt confident that she was capable to function on her Norwegian trek.
Conclusion: This patient presented with a chronic weakness in her lower back and hips that was progressively limiting her ability to walk and function most notably walking up stairs. She also had left arm pain, limited range of motion, and weakness but was most concerned about her limitation in walking due to a planned hiking vacation trip. Following 6 office visits over two weeks she had recovered good function of her legs that she felt should could confidently go on her trip and be able to fully function.
Indexing terms: Chiropractic; SOT; humeral head; radial head; Category Two blocking.
Cite: Greene M. Chiropractic care for a patient preparing for a Norwegian Trek when she couldn’t walk up stairs: A case report. [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#GreenWalkUpstairs

Michelle Greene, DC graduated from Cleveland Chiropractic College – Los Angeles in December 1992. She has been practicing in the Los Angeles area since that time. She was introduced to chiropractic as a teenager while running with the Santa Monica Track Club. She continues to compete in the aqua-bike division of Triathlons and focuses her practice on combining soft tissue work with chiropractic adjustments.
39-year-old male patient presenting with traumatic L4/5 and L5/S1 central disc herniation and stenosis conservatively treated with chiropractic care: A case report [Abstract]
Objective: To share a novel low-force chiropractic method of care that successfully treated a patient with severe low-back pain and sciatica that was resistant to surgical or epidural medical procedures.
Clinical Features: A 39-year-old male patient with a prior history of low-back pain and sciatica presented to this office with a severe aggravation of his condition secondary to a fall. He was unable to move and was taken to the ER where he was heavily medicated and sent home. Five-days later since his condition was not improving was seen at this office presenting with positive orthopaedic/neurological examination findings and MRI revealing L4-S1 disc herniations with bilateral foraminal stenosis.
Intervention/Outcome: The patient was treated 20-times over three-months with sacro-occipital technique category three pelvic block therapy, psoas myofascial release, LightMD therapy, and various cranial therapies specific for his low-back pain. After three-months the patient had negative orthopaedic/neurological findings, no sciatica, minimal low-back pain, and was able to play catch with his son.
Conclusion: Chiropractic care in this case was able to help a patient not wanting surgery or epidural injections recover function and become virtually pain free. Further chiropractic preventative care has been discussed with this patient.
Indexing terms: Chiropractic; SOT; central disc herniation; foraminal stenosis; Category Three blocking; cranial therapies.
Cite: Bloink TE, Blum CL. 39-year-old male patient presenting with traumatic L4/5 and L5/S1 central disc herniation and stenosis conservatively treated with chiropractic care: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#BloinkBlumCentralDiscHerniation
Thomas Bloink, DC, CSP, CSCP specializes in cranial-dental integration in Silicon Valley at the California Cranial Institute, which was founded in 1992. Dr. Bloink was on the board of advisors to help create SOTO USA and is actively involved in promoting the organization, presenting at research conferences throughout the world, and developing novel treatment approaches for functional neurological conditions. He works closely with many different specialists including dentists, orthodontists, and oral-maxilla surgeons. ENT's and others to ensure the best possible outcome for his patients.
Chiropractic treatment of a 47 year old female presenting with significant bilateral reduced shoulder ranges-of-motion since childhood: A case report [Abstract]
Objective: To share conservative chiropractic care for a patient presenting with virtually life-long reduced bilateral shoulder ranges-of-motion.
Clinical Features: A 47-year-old female presented to an interdisciplinary clinic for chiropractic care with bilateral difficulty raising her arms due to shoulder restrictions more than a 25° angle (flexion and abduction) since childhood. She was also concurrently suffering from daily leg and sharp pains in her legs and 'balls' of her feet.
Intervention and Outcome: Treatment consisted of sacro-occipital technique, cranial techniques and trigger point therapy to address spinal, upper extremity, and postural imbalances. After 5-months of treatments one-to-two times per week, patient reported significant improvement in shoulder ranges-of-motion with right-shoulder flexion/abduction reaching 90° and left-shoulder flexion/abduction reaching 135°. During the five-months of care the patient also has reported having no pain in her legs and feet with significant improvement in lower extremity strength and function.
Conclusion: The patient’s chronic unresponsive shoulder reduced ranges-of-motion improved for the first time since childhood with care at this office. Prior interventions included medication, physical therapy, and HVLA diversified technique chiropractic, which had no effect. She is still continuing with care, though with greater intervals between sessions, to help maintain her improvements.
Indexing terms: Chiropractic; SOT; shoulder ROM; conservative care.
Cite: Stowell LM, Blum C. Chiropractic treatment of a 47 year old female presenting with significant bilateral reduced shoulder ranges-of-motion since childhood: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#StowellShoulderROM

Lisa M Stowell, DC focuses on the safest and most natural approach to chiropractic care utilising cutting edge techniques such as SOT (sacro-occipital technique). She incorporates 'Food First' as part of her approach to customise personal dietary needs as well. Besides head, neck and low back pain, Dr Stowell addresses conditions such as diabetes, fibromyalgia and even depression and fatigue. Dr Stowell has been published in an international, peer-reviewed chiropractic journal as well as accepted for presentation at 2024 ACC-RAC Conferences.
The SOT diagnostic indicators system is a great guide for successful treatment protocols for severe physically compromised patients: A case report [Abstract]
Objective: To establish the concept that sacro occipital. technique (SOT) is a method of chiropractic which includes diagnosis and treatment through a researched specific indicator system. The advanced practitioner who understands the SOT indicator system and also has years of experience with patient application; can be creative with treatment on the very challenging cases with very physically compromised patients utilising the SOT indicator system as a guide - which may not necessarily follow normal protocols and procedures for the less compromised patient.
Clinical Features: This patient is a 69-year-old female who has had multiple lower back surgeries that have not relieved left leg and foot pain. Patient had a bad fall in February of 2022 where she fractured Lumbars 4 and 5. After the 2 surgeries to repair L4 and L5 (the second surgery to remodel the first surgery), the patient was left with both bladder and bowel incontinence as well as chronic sciatic pain in complete left leg and ankle. On evaluation the patient’s left leg and foot exhibited intermittent paralysis. The patient is on Oxycodone daily for constant excruciating pain and also had an Evoke Patient Controller (ECV by Saluda Medical, Australia) spinal cord stimulator implanted to help with pain control.
Methods: Chiropractic manipulative therapy was applied via SOT and SOT Craniopathy for evaluation and treatment. SOT Indicator system was used to establish which Category to use in treatment; in this case the patient received a mix of Category III and I. Category III treatments included orthopaedic blocking; spinal adjusting via R+ C factors; and Category III basic cranial. These were the initial few visits. After a few visits monitoring heel tension the patient required Category I treatments which included blocking, $ and/or #, SB +, vasomotor neutralisation and appropriate intra-oral cranial to free the sphenoid bone. Patient received the most pain relief from the Category I procedures.
Other evaluations included standard orthopaedic and neurological testing as well as PRO Balance 360 testing. Pro Balance 360 was used for not only evaluation but also treatment of the patient’s balance stability. The PRO Balance 360 will give a metric which represents how far the patient’s body will sway away from the patient’s centre of gravity line and is Decisional Support System certified by the United States government as the only unit currently in use at the Veterans Administration Health Care Facilities.
Results: Reevaluation after 10 visits of SOT and SOT Craniopathy utilizing mainly Category III and Category I protocols: patient has improved approximately 50%. Areas of marked symptomatic improvement: pain reduction; better quality of life: greater desire to go out and do things after each adjustment instead of going home to bed. Objective improvement illustrated Balance metric more stable; all evaluation indicators improved.
Conclusion: The SOT indicator system can be an important tool to successfully guide chiropractic treatment protocols for very challenging patient health conditions. Further research is needed to see if the results from this case can be generalised to other patient populations.
Indexing Terms: Chiropractic; SOT; Cranial; Category One; Category Three; failed low-back surgery.
Cite: Remeta E. The SOT diagnostic indicators system is a great guide for successful treatment protocols for severe physically compromised patients: A case report [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#RemataCompromised
Esther M Remeta, DC is a practising chiropractor and clinical researcher. She has practiced for over 30 years in North Carolina and is currently the executive director of Chiropractic Research Institute (CRI) in Clemmons. Dr. Remeta is a SOTO-USA Board Certified Sacro Occipital Technique and Craniopathy practitioner and a Diplomat with the American Academy of Pain Management. She is on the faculty of SOTO-USA and lectures nationally and internationally to her fellow colleagues in the field of brain and spinal cord trauma rehabilitation.
The importance of addressing the psoas muscle in sacro occipital technique’s category two and three. A commentary
Introduction: Sacro occipital technique (SOT) (1) notes that sacroiliac joint instability and hypermobility with pelvic torsion (category two) triggers a comprehensive series of compensatory mechanisms that extend throughout the musculoskeletal and neurological systems. A hypermobile pelvis alters proprioceptive input, triggering reflexive psoas contraction and heightened tension in pelvic floor muscles as the body attempts to achieve stability. (2( This muscular compensation, by way of the cerebellar visual and vestibular righting mechanism can create a defensive mechanism affecting the cervical spine and even temporomandibular joint (TMJ) dysfunction. (3-6)
The Psoas Muscle and Sacro Occipital Technique: Additionally, a hypertonic psoas major augments shear stiffness within the lumbar motion segment, altering spinal biomechanics and leading to dysfunction in both the lumbar spine [category three) and sacroiliac joint.
Category three patients commonly present with lumbar and lumbosacral discopathy, sciatic nerve radicular syndromes, and antalgic body positioning. (7) The psoas major is integral to lumbar spine stability and pelvic alignment, making it a key factor in posture, movement, and overall spinal health. While traditionally recognised as a hip flexor, its role extends far beyond simple movement. Research suggests that the psoas functions as both a stabiliser and a dynamic mover, adapting based on spinal positioning and load demands. (8)
Because the psoas muscle originates from the lumbar vertebrae (T12-L5) and inserts onto the femur, it has a direct influence on spinal alignment, sacroiliac joint stability, and hip function. Dysfunction in this muscle, whether from hypertonicity, weakness, or asymmetry - can lead to a cascade of mechanical issues in the lower back, pelvis, and lower extremities. DeJarnette the developer of SOT stated 'Category three is a result of the body’s failure to adapt to the category two'. (7)
When a category two dysfunction is not properly addressed, it can progress to category three, where more advanced compensatory patterns and structural breakdowns occur. Patients with category three presentations commonly exhibit various types of antalgic postures as a protective response to pain and instability. The psoas major, being a crucial stabilizer of the pelvis and spine, plays a central role in this process. Dysfunction in the psoas can exacerbate sacroiliac joint dysfunction, alter pelvic mechanics, and perpetuate a cycle of neuromuscular imbalance.
Conclusion: Therefore, recognising and addressing psoas function is essential in both rehabilitation and performance-based chiropractic care. In the SOT approach, restoring sacroiliac stability and reducing pelvic torsion through specific pelvic block placement and associated adjunctive protocols helping regulate the neurological and biomechanical effects of psoas dysfunction. Conversely psoas tension can occur as the body attempts to stabilize a hypermobile sacroiliac joint so treatment to reduce this compensatory tension can be important prior to pelvic block placement used to treat pelvic torsion and associated hypermobility. By integrating these SOT category pelvic block placement methods with specific psoas release and activation techniques, practitioners can effectively manage category two dysfunction and prevent its progression to category three, ultimately improving structural integrity, postural balance, and overall spinal health.
Indexing terms: Chiropractic; SOT; psoas major; Category One; Category Two; Category Three.
Cite: Wong J. The importance of addressing the psoas muscle in sacro occipital technique’s category two and three. A commentary. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#WongPsoas
Getzoff H. Sacro Occipital Technique (SOT): A Systems Driven Method of Chiropractic. Asia-Pac Chiropr J. 2024;4.4. http://apcj.net/Papers-Issue-4-4/#GetzoffSOTSystem
Mank VM, Barranco-Trabi J, Mank JK, Roberts J, Newman DP. A Case Study of Chronic Iliopsoas Tendinopathy and Sacroiliac Joint Dysfunction Masquerading As Pelvic Girdle Pain. Cureus. 2021 Jun 17;13(6):e15719. https://pubmed.ncbi.nlm.nih.gov/34290919/
Morningstar MW, Pettibon BR, Schlappi H, Schlappi M, Ireland TV. Reflex control of the spine and posture: a review of the literature from a chiropractic perspective. Chiropr Osteopat. 2005 Aug 9;13:16 https://pmc.ncbi.nlm.nih.gov/articles/pmid/16091134/
Fink M, Wähling K, Stiesch-Scholz M, Tschernitschek H. The functional relationship between the craniomandibular system, cervical spine, and the sacroiliac joint: a preliminary investigation. Cranio. 2003 Jul;21(3):202-8 https://pubmed.ncbi.nlm.nih.gov/12889677/
Gregory TM. Temporomandibular disorder associated with sacroiliac sprain. J Manipulative Physiol Ther. 1993 May;16(4):256-65. https://pubmed.ncbi.nlm.nih.gov/8340721/
Panahpour A, Blum CL. TMD - Chiropractic and Dentistry: Two case reports. Asia-Pac Chiropr J. 2025;5.4. www.apcj.net/papers-issue-5-4/#PanahpourBlum
Getzoff H. Sacro Occipital Technique (SOT): Category Three: Predictability of Outcomes. Asia-Pac Chiropr J. 2024;4.3. apcj.net/Papers-Issue-4-3/#GetzoffSOTCat3
Sajko S, Stuber K. Psoas Major: a case report and review of its anatomy, biomechanics, and clinical implications. J Can Chiropr Assoc. 2009 Dec;53(4):311-8. https://pmc.ncbi.nlm.nih.gov/articles/PMC2796950/

Jacky Wong DC is a recent graduate from Life Chiropractic College West, Class of 2024. He has a special interest in Sacro Occipital Technique (SOT), a gentle and versatile method that allows him to care for patients of all ages. Passionate about serving underserved communities, he is particularly dedicated to supporting children’s developmental growth through chiropractic care. Dr Wong is committed to making holistic, patient-centered care accessible to those who need it most.
Major B De Jarnette, DO, DC. Founder and Developer of Sacro Occipital Technique
Narrative: Dr. De Jarnette was a pioneer in the early times of chiropractic. He devoted his life to trying to understand the complexity of the human body. His analytical lens was 3-fold, utilising engineering, osteopathic, and chiropractic concepts. His education and early times in chiropractic research allowed De Jarnette to develop a base of chiropractic knowledge that would be tough to duplicate by one person today.
His concept was to develop a way to functionally read a patient’s physiological presentation to treat patients more efficiently. He realized the patients he treated had similar biomechanical dysfunctions and associated indicators. These dysfunctions and indicators would be the foundation of his category system approach to patient care. The categories, originally 21 and narrowed to 3 basics, represented dysfunction in critical areas of patient physiology:
Category 1 relating to a patient’s CSF circulation ability/dysfunction
Category 2 was a foundational fault relating to instability/hypermobility of the SI joint complex
Category 3 was essentially our limitation of matter, resulting in lumbar disc herniation with associated sciatica.
De Jarnette was born on December 23, 1899, and raised in Nebraska. After high school, he accepted a scholarship as an apprentice in experimental engineering. In 1918, he moved to Detroit to work as a design engineer at Timken Detroit Axel Co. While working at the company, He was injured in a boiler explosion that killed 5 of his coworkers. Severely injured and unable to continue working, he sought osteopathic care for his condition. Treatment for his injuries consisted of spinal and cranial therapies. Dr Garner Sutherland, DO, considered the founder of cranial osteopathy, personally treated him.
While receiving care, De Jarnette decided to pursue a DO degree. He attended Dearborn College of Osteopathy located in Elgin, Il. Dr Charles H Murray DO founded the college in 1912 out of his home based on his osteopathic textbooks. Murray ran the college with faculty assistants and considered building a college from that. De Jarnette graduated from Dearborn in 1922.
After receiving his degree from Dearborn, Dr De Jarnette returned to Nebraska. While in Lincoln, he met with Dr NB Crabtree, president of the Nebraska College of Chiropractic. Crabtree encouraged De Jarnette to further his education and acquire his DC degree in 1924. De Jarnette opened his practice in Nebraska City, Nebraska, in June 1925. His practice was located above The Farmers Bank and would be where he continued to develop his queries in chiropractic.
With this unique education, he spent the rest of his life developing his technique and helping people. Over his chiropractic career, he authored over 135 volumes of information on his technique.
DeJarnette’s path to becoming a chiropractor is interesting and gives valuable insight into his methods of developing the Sacro Occipital Technique.
Indexing terms: Chiropractic; SOT; De Jarnette; DeJarnette; History.
Cite: Hagen C. Major B De Jarnette, DO, DC. Founder and Developer of Sacro Occipital Technique [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#HagenDeJarnette

Chad Hagen, DC is is a 2005 Palmer graduate and second generation chiropractor. Classically trained in Atlas Orthogonal and a Certified SOT® Instructor, Dr. Chad’s private practice specializes in these techniques located in Bettendorf, Iowa. As Assistant Professor at Palmer Davenport, Dr. Chad teaches in both the Technique and Philosophy Departments. His instructional focus is Subluxation Analysis, Toggle Recoil, Chiropractic Theory, and both the Sacro-Occipital Technique electives. Dr Hagen is also Advisor for the SOT and Palmer Upper Cervical clubs.
Has the field of chiropractic discarded 'healing touch' as part of its armamentarium? Reiki, a literature search, and its implications for the chiropractic profession. [Abstract]
Objective: Chiropractic, founded by D. D. Palmer a magnetic healer, is entering into the evidence-based healthcare arena and concurrently is attempting to integrate into the biomedical field. Chiropractic’s academic community has therefore attempted to distance itself from touch and its healing energetic capacity. Ironically Reiki (healing touch) has been flourishing within the biomedical community, however does it have an evidence base?
Methods: A search of PubMed for 'Reiki' in the title of an article was performed and articles were reviewed for this method’s application in the biomedical community.
Results: 201 articles were retrieved and of those articles evidence supportive of Reiki (healing touch) were found: Oncology (23-studies), Hospital Setting (13-studies), Pediatrics (11-studies), Nursing (15-studies), HIV (2-studies), COVID (4-studies), Pain Relief (23-studies), Psychotherapeutic Applications (21-studies), Animals (3-studies), Female Focused (2-studies), Cardiovascular (5-studies), and Placebo Comparative Studies (4–studies).
Conclusion: It is interesting that while many researchers in the chiropractic field are attempting to eliminate any discussion of 'healing touch' from the chiropractic encounter, Reiki is embracing this concept and gaining biomedical acceptance. Chiropractic is a hands-on method of healing and the Reiki research supports considering investigating the value of healing touch within the chiropractic field.
Indexing terms: Chiropractic; SOT; Reiki; Healing touch.
Cite: Blum CL. Has the field of chiropractic discarded 'healing touch' as part of its armamentarium? Reiki, a literature search, and its implications for the chiropractic profession [Abstract]. Asia-Pac Chiropr J. 2025;6.2. www.apcj.net/SOT-Abstracts-2025/#BlumReiki
Charles L Blum DC, CSCP is in private practice Santa Monica, California and past president of SOTO – USA, now their research chair. He serves as Adjunct research faculty at Cleveland Chiropractic College and associate faculty at Southern California University of Health Sciences teaching the SOT Elective. Dr. Blum is a Certified SOT Cranial Practitioner, and on the peer review board of the Journal of Craniomandibular and Sleep Practice (CRANIO), Association of Chiropractic College Conference Peer Review Committee, Journal of Contemporary Chiropractic, Asia Pacific Chiropractic Journal, and Journal of Chiropractic Medicine. He has lectured nationally and internationally, has written various SOT related texts, compiled SOT and cranial related research, and has extensively published in multiple peer reviewed indexed journals and at research conferences from 1984 to the present.